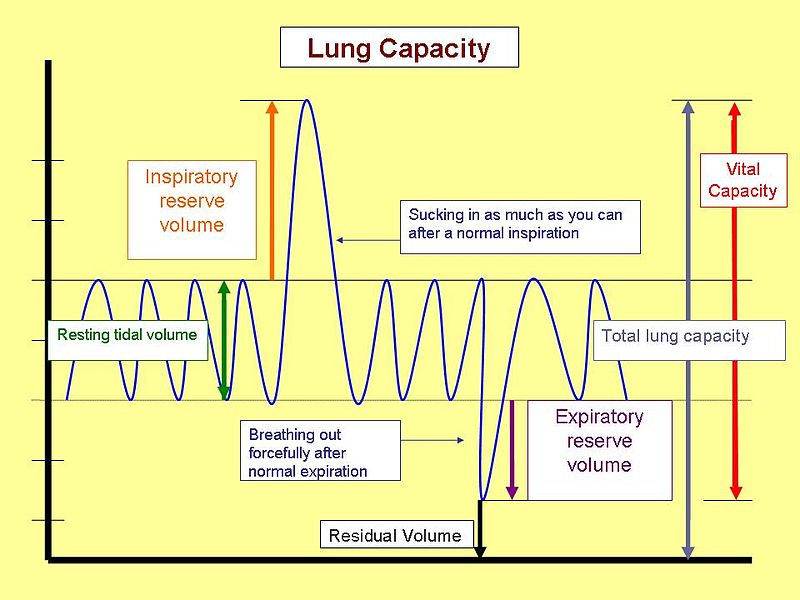
The vital capacity is the volume of gas that can be exhaled by a maximal expiration from total lung capacity.
Control of Ventilation and Respiratory Muscles
Vital capacity (VC) is easily measured with spirometry; decreases in VC point to respiratory muscle weakness. The VC averages approximately 50 mL/kg in normal adults. VC changes are not specific, however, and decreases may result from both inspiratory and expiratory muscle weakness and may be associated with restrictive lung and chest wall diseases. A marked fall (of greater than 30%) in VC in the supine compared with that in the erect posture (which in the normal person is 5% to 10%) is associated with severe bilateral diaphragmatic weakness.
Vital capacity is reduced by 25% to 50%, and residual volume increases by 13% following many general anesthetics and surgical procedures. Upper abdominal incisions and thoracotomy affect pulmonary mechanics the greatest, followed by lower abdominal incisions and sternotomy. Expiratory reserve volume decreases by 25% after lower abdominal surgery and 60% after upper abdominal and thoracic surgery. Tidal volume decreases 20%, and pulmonary compliance and functional residual capacity decrease 33%. Atelectasis, hypoventilation, hypoxemia, and
pulmonary infection may result. Many of these changes require a minimum of 1 to 2 weeks to resolve.
Difference Between Forced Vital Capacity and Vital Capacity
Forced Vital Capacity vs. Vital Capacity
In
spirometry, the default basis for the assessment, monitoring, and diagnosis of chronic obstructive pulmonary disease (COPD) requires a device called a spirometer. This is to help predict the hyperinflation with obstruction of airflow in patients with this kind of disease, thus saving lives. A spirometer is a device used by health professionals to measure timed, inspired, and expired volumes. From these volumes we can derive how quickly and efficiently the lungs can be filled and emptied. The spirometer was created in 1846 by a man named Hutchinson. Its basic use is to measure ventilatory function – the dynamic volumes of the lungs and the maximal rates of the flow. This is very important because spirometry may help in the analysis of asthma, and it can also supply information on the analysis of other reasons for dyspnea.
There are different kinds of measurements made with the spirometer. One of these is vital capacity – the highest level of air volume a device can exhale or inspire during a forced vital capacity (
FVC) or a slow vital capacity (VC) maneuver. All of these measures are used to determine the measurement of a ventilatory function. There is a lot that can be learned regarding the mechanical properties of the lungs using the data gathered from the measurements of forced maximal inspiration and expiration. Two types of blows are done: the first is the “relaxed” slow vital capacity (VC), followed by forced vital capacity (
FVC). Air becomes trapped when there is a significant difference between VC and FVC.
VC starts with full inspiration. The patient blows out in a very slow and relaxed manner similar to a heavy and deep sigh, which is done until the lungs are fully emptied. There should be at least three blows, at least two of which should be within the range of 5% or 100mls.
FVCalso starts with full inspiration. After this, the patient blows out very fast and hard until the lungs are completely empty. Three blows should be done, wherein at least two should be within the 5% or 100mls scale. A volume plateau should be reached while blowing in the volume time graph, which may take over 12 seconds for people with a very severe case of COPD.
According to most studies, a minor difference in vital capacity occurs in healthy individuals if the forced maneuver is opted for instead of the slow maneuver. On the other hand, this diffirence is far greater in patients with a case of airflow obstruction, wherein the difference elevates in proportion to the degree of obstruction.
Summary:
1. In spirometry, the default tool for the assessment, monitoring, and diagnosis of chronic obstructive pulmonary disease (COPD) is a device called a spirometer.
2 .A spirometer is a device used by health professionals to measure timed inspired and expired volumes.
3. There are different kinds of measurements made with the spirometer; one of these is vital capacity, which is the highest level of air volume a device can exhale or inspire during a forced vital capacity (FVC) or a slow vital capacity (VC) maneuver.
4. Two types of blows are done; the first is the “relaxed” and slow vital capacity (VC), followed by forced vital capacity (
FVC). Air becomes trapped when there is a significant difference between VC and FVC.
5. According to most studies, a minor difference in vital capacity occurs in healthy individuals if the forced maneuver is opted for instead of the slow maneuver.